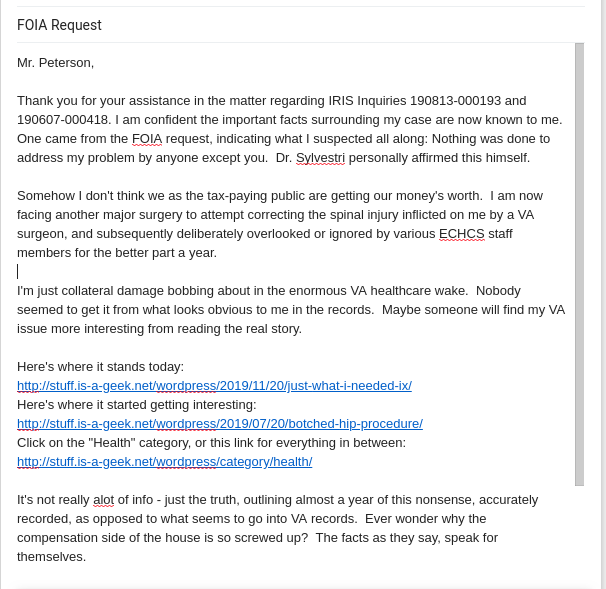
Specific VA personnel issues pertaining to my case appear below. Several things called out with an *asterisk, are directly quoted from official VA records.
A. To the forgetful Post-Op nurse: Before “not wanting to wake up” the patient to bring medication on schedule, review the Doctor’s orders and improve your understanding of basic pharmacology regarding the specific medications you are dispensing. Do not allow patients to slip into excruciating breakthrough episodes. Failing that, when they do wake up screaming from the pain running up and down their spine, for example (not the hip) annotate the record, if you can find the time at 3 o’clock in the morning. Remember arguing about the numbers when the patient said “OK then, it’s a 10?” Your career is coming to a close soon if this isn’t the last wake-up call like this you get.(LATE UPDATE LATE 2022: It would now seem this was their 1st attempt to take me completely out of the picture, obviating any need for accountability or claims processing)
B. To the Physical Therapist who noted: “*Pt reports he feels like he has a bag of cement around his pelvis” The term used was concrete underpants. It’s still being used today. In one ear, out to the computer incorrectly and done isn’t working. The hip twisting was a bad idea, too. Patients coming apart with back injuries don’t like it. Hip surgery patient with the opposite side of their body so contorted from muscle clenching it makes that leg a half inch shorter, are a “bad” thing. Why they might feel compelled to make their own lift shoe in order to be able to walk, is another big, red flag. You might be in the wrong line of work.
C. To the Primary Care Physician who observed: “Sometimes it just takes longer to get over an operation.” Contrary to ECHCS rumors these days, the human body heals at relatively consistent rates, based on age, nutrition and other factors. Patients with unexplained issues need a call made. You seem to be pushing them in the wrong direction. Consider working on the listening skills if you have any plans for career advancement.
D. To the PA who observed: “We don’t usually see this on the right side after a left hip replacement.” Take some Ibuprofen and come back in a couple months is not the correct response to that situation. The email saying “*he can go to the ER.” can be particularly insulting, under these circumstances. But it did get into the record, so 2-for-2 on the keyboard skills. Knowing the ER is not a real option, making a good rabbit hole to throw somebody down only makes more futile work for the ER. Avoiding work is not what we do here. You are in the wrong line of work.
E. To the Surgeon who remarked: “I’ve done many of these procedures and never saw anything like this before.” Many people drive up and down I-25 for years and never get in a car accident. What does either of those things have to do with “my” surgery recovery? Your education didn’t stop when you got your license to practice. That’s what we’re calling this one: a “practice” session. Much better attention to detail will be needed, going forward. One of your colleagues inadvertently gave you up. This either was or will be, your last chance.
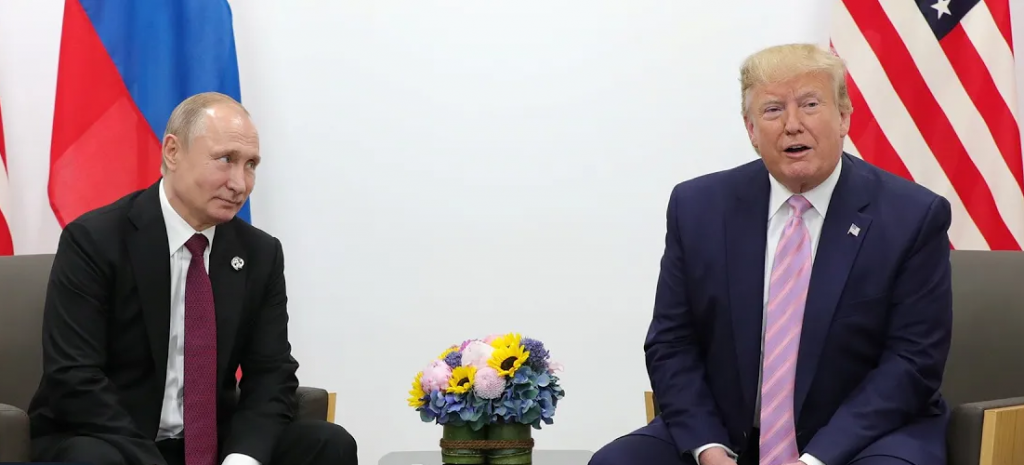
F. To the rehab doctor who quipped: “Since January, huh? Looks like it’s chronic now.” Your medical opinion is the only thing that matters. We have an idiot in the Oval office now because of what things “look like.” You got it wrong, demonstrating inappropriately presumptuous hubris, failure to read and understand the records, and failure to read and listen to the patient. Your job was literally done for you, and you still turned it down. You are in the wrong job.
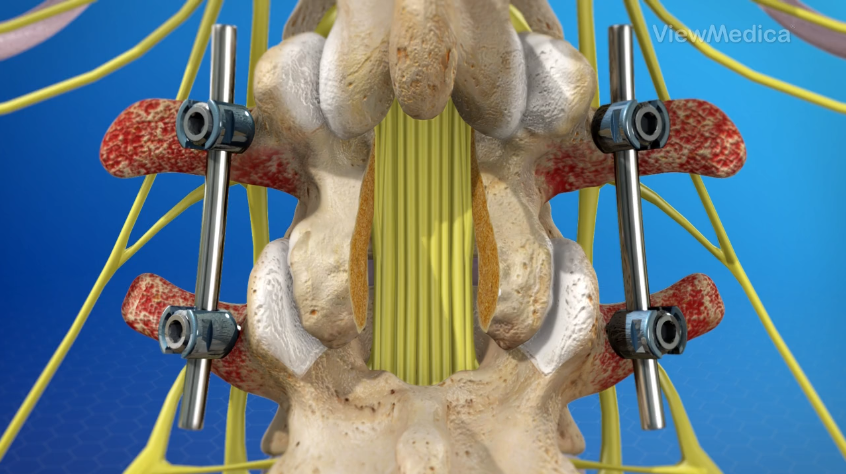
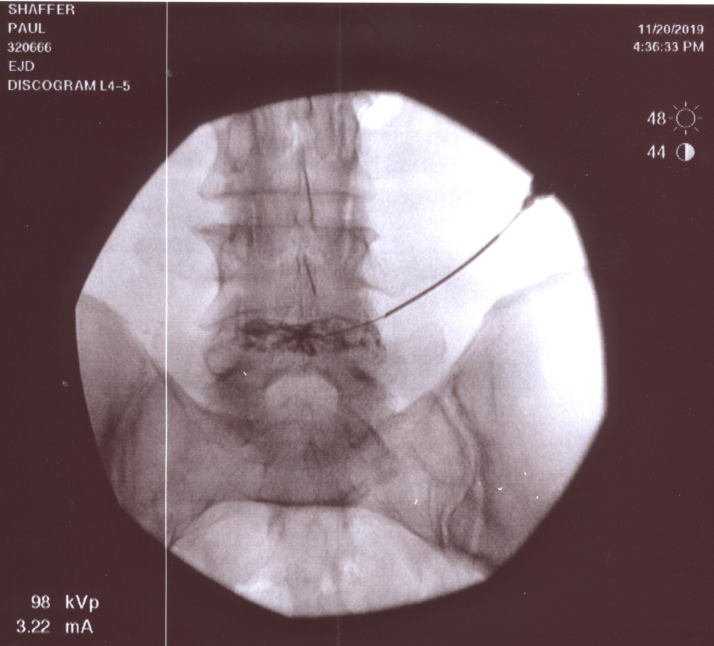
G. To the Joint Doctor who noted: “…*thinks he got a back injury…” Yes, they certainly do think about that all the time, when they are injured. But it’s mostly a feeling – pain inflicted by one of your doctors, in this case. Here’s what the record said about what the patient “thought:” “*Mr. Shaffer has had low back pain that got worse after his hip replacement.” An open-ended therapeutic misadventure for the patient is ongoing to this day due in large part to your failure to recognize and properly refer the case. Your PA might remember shuffling them out of the exam room literally yelling “I can’t walk with this shit!” Comprehend the message left with you the day you met that man, as well as the one left here now – for the benefit of your next patient.
H. To the Chief of Orthopedics who replied: “*I don’t see any delay in care from the orthopedic point of view…” That seems to be an issue for almost everybody addressed here, right down the line – seeing any problem at all. Did nobody want to see the back injury? Or want to even admit the patient had a serious back injury? People reading the record can’t not see it. Is there a filtered “from the orthopedic POV,” only you see? The record tells a different story. Characterizing the symptoms expressed all along as anything “normal” is absurd.
Now that everybody is on the same page with the blanks filled in a year later, what is your definition of the term “delay” in this context? The patient is still stumbling around crippled a year later. Can you explain why the MRI he literally demanded in June did not happen in January? We already know how he slipped through the PA net under your direct purview for 3 months. Any indication what the problem there might be, in your orthopedic POV? Your cursory dismissal of his complaint effectively sentenced him to an ongoing year of misery and frustration. How many others like him out there? Any of them still alive, Chief?
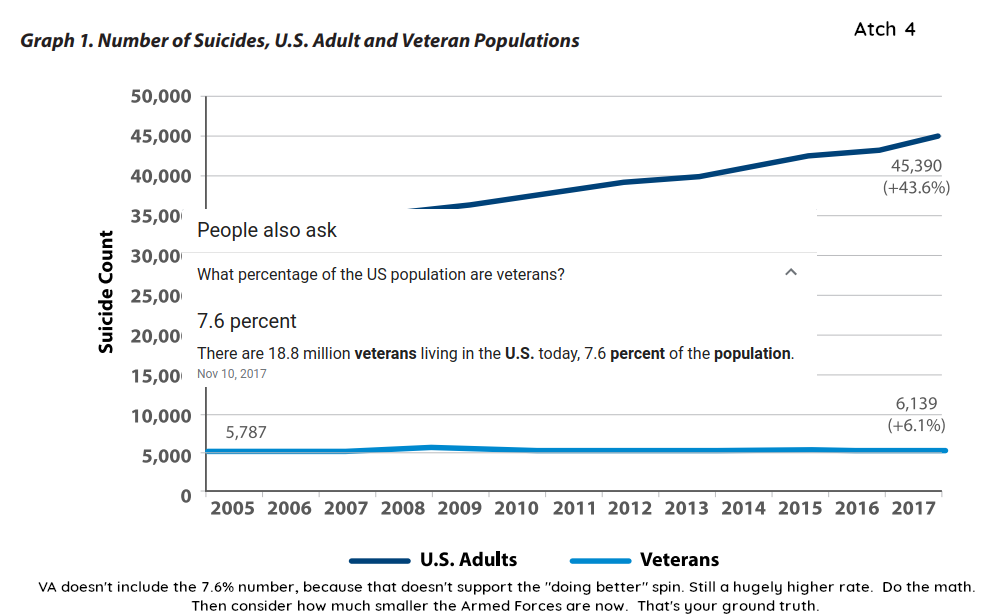
In a nutshell: You took a disabled vet, disabled him some more, rubbed it in, flatly refused to diagnose and treat, driving him to the brink of suicide as he unsuccessfully sought help from a healthcare system ignoring his pleas.
Fair criticism? I look forward to speaking with people interested in exploring this narrative further, in detail, fact or general intent. Big suicide prevention push going on lately, I hear. Now you know all about how that works for me. Push this. On the inside. I mean that literally – inside of who or whatever you think might have a relevant problem inside of it.